Published in Medical Writing 2012 Vol. 21 No. 4; 8(19):305-307
Improving patient communication by writing with empathy
Medical writers’ texts are either written for specialists or for non-professionals such as patients and their relatives. Medical writers whose work is intended for patients cannot merely impart facts. They also need to demonstrate that they comprehend the patient’s emotions – they must write with empathy. Empathic texts are intelligible, credible, and are written from the patient’s perspective. They can help patients realistically appreciate their situation and assess the advantages and disadvantages of different therapy options. In this way, empathic writing can promote health-conscious behaviour and can foster treatment adherence.
Introduction
Medical writers’ texts are usually directed toward specialists such as licensing authorities or the scientific community. Increasingly, though, medical writers also find themselves writing for nonprofessionals, including patients and their relatives, because decisions regarding diagnostic procedures and treatment are no longer made exclusively by physicians and therapists. In the digital and print media, patients search for and find information about pharmaceuticals and medical procedures and – armed with this knowledge – seek out clinics and medical practices that offer what they feel best fits their needs. Texts written for the purpose of patient communication can help them to realistically appreciate their situation and assess the advantages and disadvantages of the various therapy options.
Successful patient communication is especially crucial in cases of chronic illness, which result in complex, regular treatment routines over an extended period of time. Furthermore, in some situations, treatment becomes the responsibility of the patients themselves. In such cases, effective patient communication can contribute to more health-conscious behaviour. This also fosters adherence, a factor that is often decisive for a therapy’s efficacy, because patients will only adhere to the treatment plan when they accept the need for the regimen, understand how to deal with medicines and medical application devices, and are prepared for possible side-effects.
Medical writers whose work is intended for patients cannot merely impart facts, but they also have to demonstrate that they comprehend the patient’s emotions and rationale – they have to write with empathy. That is, they have to be able to put themselves in the patients’ place, have sensitivity about their symptoms, and understand their hopes and fears. But how can this be achieved linguistically? It is certainly not necessary to follow the example of Gustave Flaubert, who purportedly experimented with rat poison to be able to write the arsenic scene in Madame Bovary. In our article, we present the principles of empathic texts, that is, intelligibility, the patient’s perspective, and credibility (Fig. 1).
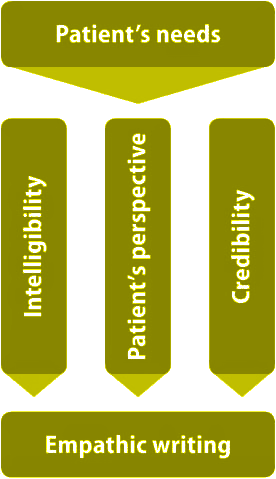
Figure 1: Principles of empathic texts.
Intelligibility
Intelligibility is without doubt the fundamental requirement of an empathic writing style because failure to reach patients intellectually precludes engaging them emotionally. This means that empathic texts for patients avoid foreign terminology, frequent exchange of synonyms, and abbreviations. Technical terms should be replaced by common terms or paraphrased in simple words. Patient-oriented texts consistently employ a single sentence to explain each important piece of information and thus transmit the knowledge in small steps so as not to overwhelm the reader. A study on the use of information booklets about cancer revealed that the information needs of patients can only be adequately met if texts are written in plain English.1 Furthermore, research has shown that text comprehension can also be facilitated by a descriptive, lively language that uses many verbs and replaces abstract formulations like ‘minimally invasive technique’ with imagery such as ‘keyhole technique’.2
Assuming the patient’s perspective
Once the condition of intelligibility is met, there are techniques that help express empathy linguistically. The simplest is to take the patient’s position: Instead of writing ‘physicians explain the therapy options’, write, ‘Patients inform themselves about possible types of treatment’. The author thus attempts to capture the patient’s situation not only linguistically, but also in the content. This can be accomplished only if the writer constantly reflects on how patients might perceive a concrete situation, that is, what the patient actually sees, hears, and feels. The simple fact that a medicine is to be administered under local anaesthesia can be expressed, ‘You will barely feel the injection because the spot will be numbed beforehand’.
The patient’s vantage point
Certainly, a healthy person requires a high degree of psychological dexterity to be able to empathize with patients experiencing an illness and all its facets. The illness’s direct symptoms or the effects and sideeffects of the treatment might not be the patient’s principal issue; often the patient’s fears or problems indirectly associated with being ill or with the treatment will be more of a concern. These fears and problems may concern relationship issues, social interactions, work, physical activity, and mobility.
Accessing self-help groups or relevant Internet forums can help writers comprehend what really disturbs the patients.
This understanding will be clear to the reader of an empathic text, particularly from the word choice. The fact is that even individual words not only convey information, but they also awaken associations. Anyone who suffers from migraines describes them like ‘attacks’ or ‘thunderstorms in my head’, and a person with a toothache refers to it using words like ‘intense’ or ‘throbbing’. Generalizing in a text about ‘pains’ or even ‘complaints’ in such cases would hardly demonstrate empathy.
Credibility
Authors striving to be perceived as empathic must be absolutely credible; they need to entirely and explicitly explain facts based on the latest medical knowledge. Explaining research results plainly yet precisely is surely one of the greatest challenges of empathic writing. Moreover, writers need to keep in mind that today’s patients want to construct their own image of the illness, prognosis, and therapy alternatives. Many patients refuse to rely on only a single authority, preferring to do their own research and compare sources; thus, patient communication texts must provide references. The vague claim that a diagnostic procedure is ‘based on scientific findings’ or that a drug ‘has been tested in clinical studies’ is definitely inadequate.
Discussion
Empathic texts should be written from the patient’s point of view. They also must be understandable and credible. In numerous ads and websites, companies and clinics describe themselves as ‘patientoriented’ or proclaim that they practice a ‘holistic healthcare approach’. We believe, however, that proving that these claims are more than platitudes can only be achieved through empathic action, that is, with empathically written texts. Only in this way – of course followed up by true empathy in physical dealings – can real proximity to the patient be achieved.
Thus, patient communications should be based on the ideal of the helpful, empathic caregiver. Empirical investigations prove that the patients’ satisfaction with their care is determined by how the physician communicates.3 Empathy can even influence the results of therapy. For example, patients recover faster from the flu when they have an empathic physician.4 On the other side of the coin, insufficient empathy impedes contact with the patient; visits that are not empathic last longer and tend to be frustrating for both the doctor and patient.5 The same may be true for patient texts: When patients understand the content and can identify with the language used, patient texts can fulfil their true function. When this happens, patients find it easier to comprehend and come to terms with their situation, accept their condition, and assess the advantages and disadvantages of the various treatment options. Finally, empathic texts can encourage health-conscious behaviour and foster compliance with the therapy plan.
1. Butow P, Brindle E, McConnell D, Boakes R, Tattersall M. Information booklets about cancer: factors influencing patient satisfaction and utilization. Patient Educ Couns 1998;33(2):129–41.
2. Langer I, von Schulz F, Tausch R. Verständlichkeit in Schule, Verwaltung, Politik und Wissenschaft [Intelligibility in Schools, Administration, Politics, and Science]. München, Basel: Ernst Reinhardt; 1974.
3. Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract 2002;15(1):25–38.
4. Rakel D, Barrett B, Zhang Z, Hoeft T, Chewning B, Marchand L, et al. Perception of empathy in the thera- peutic encounter: effects on the common cold. Patient Educ Couns 2011;85(3):390–7.
5. Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA 2000;284(8):1021–7.